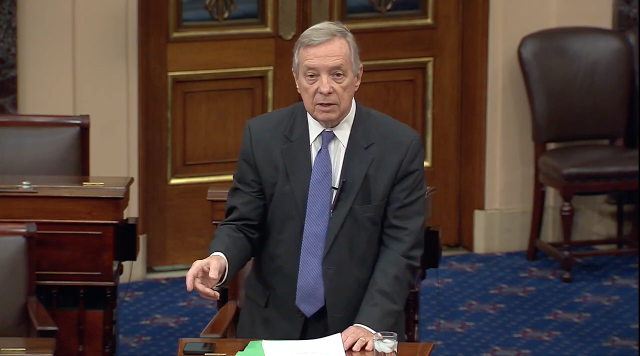
WASHINGTON – U.S. Senate Majority Whip Dick Durbin (D-IL) today sent oversight letters to three companies – DentaQuest, Envolve, and Avesis – that administer dental benefits for Medicaid managed care companies (MCOs) in Illinois to seek answers on barriers to providing dental care to Medicaid enrollees. Durbin’s letters raise concerns and investigate certain insurance practices that can limit and discourage provider participation in Medicaid, which exacerbate existing reimbursement rate challenges, resulting in an estimate of only 24 percent of Illinois dentists accepting Medicaid. As a result, Medicaid enrollees, including children and people with disabilities, have difficulty accessing adequate dental care—often facing extensive wait lists for necessary treatment.
Get The Latest News!
Don't miss our top stories and need-to-know news everyday in your inbox.
“I write today regarding significant challenges that oral health providers are facing in their engagements with Medicaid managed care organizations (MCOs) in Illinois, which is hampering patient access to this essential health care. In particular, my office has been made aware of certain practices that appear troubling and result in arbitrary or unnecessary barriers for oral health care providers in Illinois, particularly those treating children, people with disabilities, and low-income patients,”Durbin wrote in the letters.
Durbin first noted that the time-consuming process of obtaining credentialing with MCOs deters dental care providers from accepting patients enrolled in Medicaid.
“After obtaining state licensure, dentists in Illinois who want to treat Medicaid patients must enroll with the Illinois Medicaid Program Advanced Cloud Technology (IMPACT) program run by the Illinois Department of Healthcare and Family Services (HFS), which can take months on its own. But upon completion of that IMPACT step, prospective Medicaid providers are then forced to wait several additional months—compared to the timeline with PPO plans—before becoming fully enrolled and credentialed Medicaid providers,” Durbin wrote. “Long wait times to begin seeing Medicaid patients that are aggravated by MCO policies could discourage these providers from working in a federally qualified health center or other population health setting.”
Durbin continued on, explaining that arbitrary limitations on appointment length, coupled with prior authorization requirements, can prevent dental care providers from being sufficiently reimbursed. This contributes to the unacceptable wait lists—up to a year long, or beyond—for patients to receive specialized treatment, such as dental surgery under anesthesia.
“Oral health providers have shared instances of arbitrary restrictions on the time of care that MCOs would reimburse for their services. For example, anesthesia services for complex pediatric cases often require several specialized staff and implicate patients with special needs or behavioral challenges, and require multiple services and surgical intervention. These services often require two and a half hours (10 increments of 15-minutes) of anesthesia or more, yet data from more than 100 cases at a single provider indicate that MCOs in Illinois are capping reimbursement at significantly shorter increments of anesthesia,”Durbin wrote. “An apparent practice of MCOs not reimbursing for the full amount of medically necessary services rendered jeopardizes access to care for this vulnerable population.”
Providers have also hit roadblocks in having legitimate claims accepted by Illinois MCOs. Significant resources in dental care offices are spent responding to claim rejections or convincing MCOs to cover legitimate claims, dissuading providers from accepting patients enrolled in Medicaid.
“Providers have reported extensive delays in obtaining reimbursement and arbitrary rejections of qualified, legitimate claims—necessitating extensive staff time for appeal. Several studies have shown that these administrative burdens contribute to lost revenues, discourage providers from accepting Medicaid, and pull them away from their primary focus: providing essential treatment to low-income Americans,” Durbin continued.
Durbin reminded the companies that patients, including children, are suffering when MCOs put barriers in between patients and essential treatment by dental providers. In Illinois, only 37 percent of children covered by Medicaid actually have a dental visit in a given year. One recent study found that privately insured children in Illinois had six times greater odds of obtaining an appointment than children in Illinois who are enrolled in Medicaid.
“If oral health providers—already facing challenging reimbursement rates—are forced to jump through burdensome, unjustified bureaucratic hurdles to furnish care and obtain timely reimbursement, patients suffer,”Durbin wrote.
Durbin concluded his letters by asking each company a series of questions, ranging on topics from credentialing dental care providers, approving treatment claims, and coverage for dental surgery procedures.
A copy of the letter to DentaQuest is available here.
A copy of the letter to Envolve is available here.
A copy of the letter to Avesis is available here.
DentaQuest, Envolve, and Avesis together administer Medicaid dental benefits on behalf of Aetna, BlueCross Blue Shield, CountyCare, Molina, and Meridian’s MCOs.
More like this:
